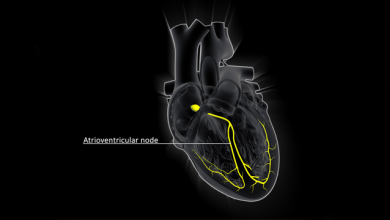
Cardiac pacing is a well-established therapeutic tool improving the survival and quality of life in patients. Indications for permanent cardiac pacing include sinus node dysfunction, intermittent and incomplete atrioventricular block, and bundle branch block.
Cardiac pacing, in conjunction with beta-blocker therapy, can potentially reduce the risk of bradycardia-dependent QT prolongation, decrease heart-rate irregularities and reduce repolarisation heterogeneity.
Cardiac resynchronisation therapy (CRT) with biventricular pacing is an effective therapy in patients with advanced heart failure (HF) – New York Heart Association (NYHA) Class III or IV, an ejection fraction (EF) 120 ms.
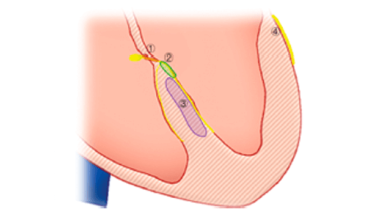
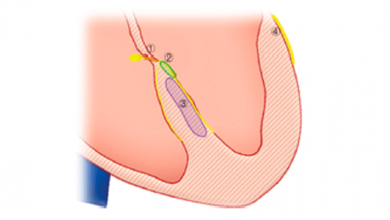
CRT has also been shown to be effective for the prevention of HF in relatively asymptomatic patients with wide QRS. However, CRT is underutilised among eligible patients. Approximately one-third of patients do not respond to CRT due to various factors, including anatomic difficulties and suboptimal lead placement. To increase the effectiveness of CRT, it has been hypothesised that pacing at multiple left ventricular (LV) sites may provide more effective resynchronisation.
In clinical studies, use of MultiPoint pacing in HF patients undergoing CRT has been associated with increased haemodynamic and clinical benefits compared with conventional pacing, particularly in patients with the least improvement from biventricular pacing.